Research activity
All current activity on heart valve disease
All current activity on heart valve disease
[wpseo_breadcrumb]
Selected Research Activity
The Valve Study Group has a number of themed research interests.
Denise Parkin, Anna Hayes, Karine Grigoryan, Chantel Lui, Ronak Rajani, John Chambers
One of our primary interests is in the optimization of care for patients with heart valve disease. This has entailed the development of sophisticated valve clinic models which brings together multiple experts in heart valve disease to deliver care to patients. From service to design to comparison against non-specialist clinic models, our work has set the framework for international guidelines.
Dr Karine Grigoryan, Dr Ronak Rajani
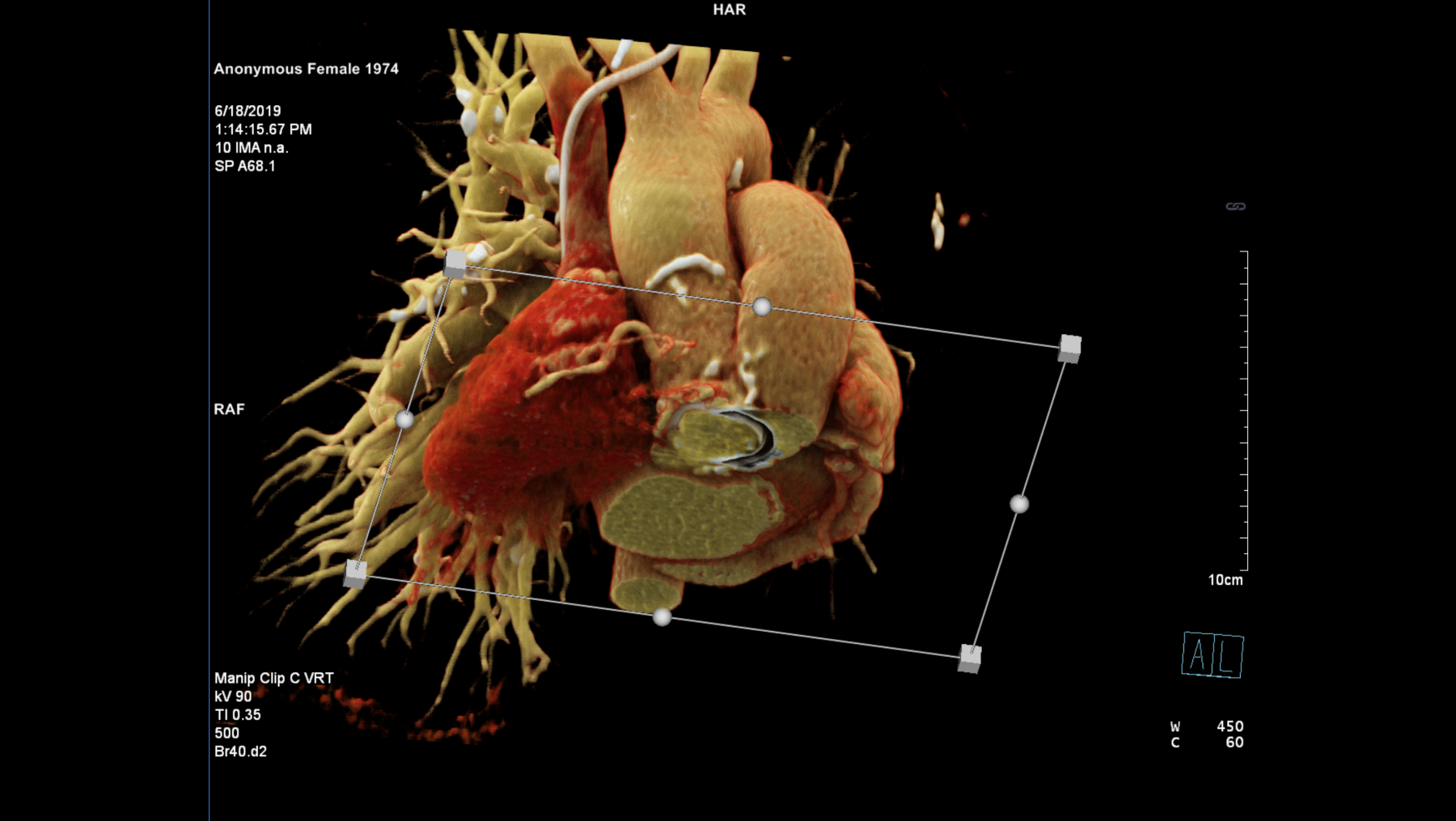
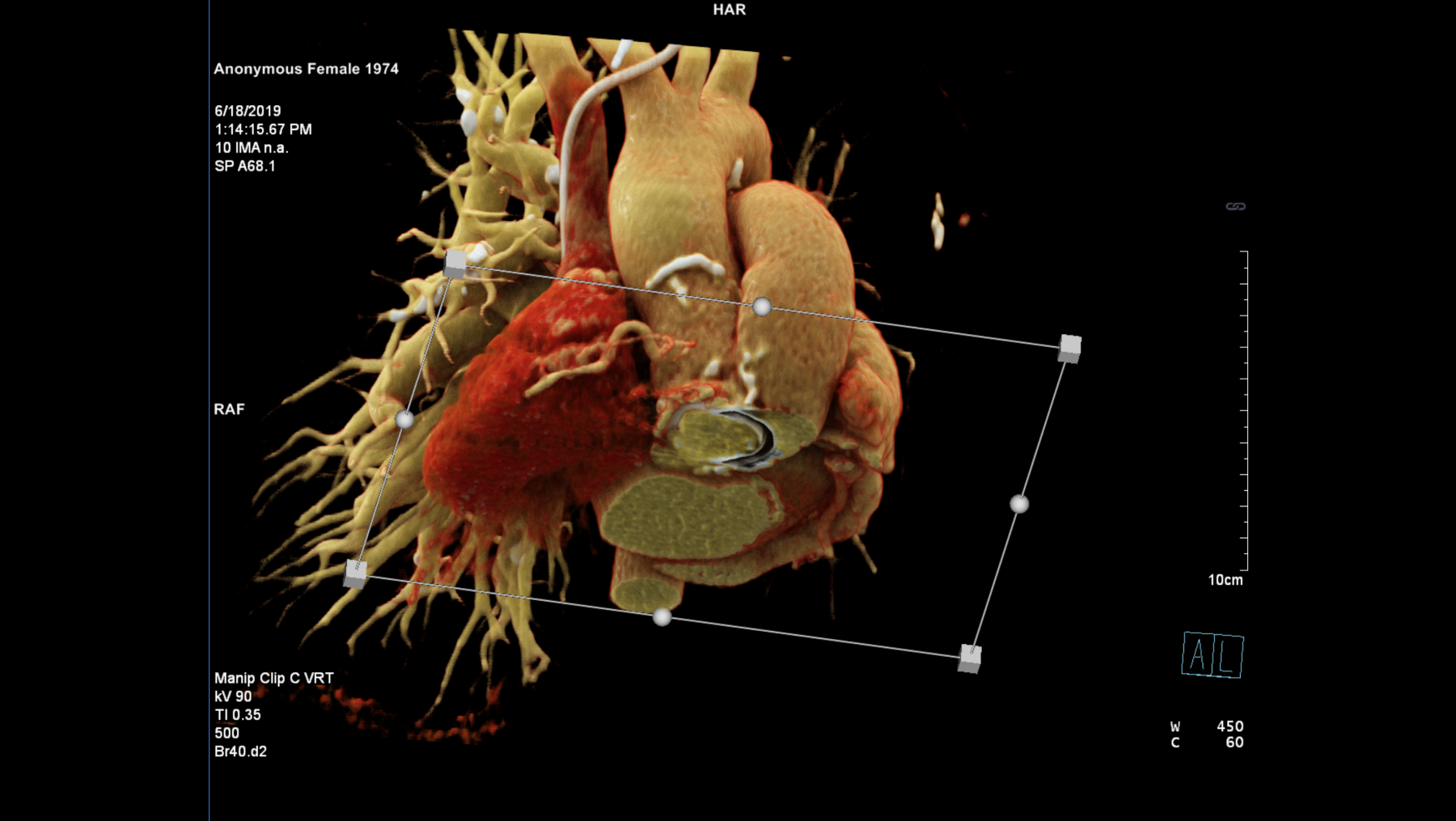
Structural heart interventions require detailed planning with echocardiography and cardiac computed tomographic angiographic studies. In order to enable patients to achieve the best possible outcomes we are investigating novel techniques to enhance procedural guidance. This extends from improving the workflow with existing imaging modalities to working with our bioengineering colleagues at King’s College London to develop new techniques for complex valve intervention planning. We also have existing projects with industry partners to help develop pre-procedural computer simulations and also to enable imaging data to be fused in real time for our interventional cardiology colleagues.
The valve study group has a long-standing interest in investigating the natural history of valvular heart disease with a particular emphasis on aortic stenosis. Data collected by our group was instrumental in ratifying the use of exercise stress testing for evaluating symptoms in patients with aortic stenosis. Our ongoing work in this area has revealed new parameters for better predicting symptom onset from physiological testing, blood biomarkers and tests for arterial stiffness. Recently we have turned our attention to different valve disease states such as tricuspid regurgitation and mitral regurgitation with the hope to better understand how these conditions progress and what factors influence survival.
As well as refining existing technique for evaluating heart valve disease, our group is developing cutting edge technologies to evaluate heart valve disease using cardiac magnetic resonance imaging techniques. The group is currently collaborating with Dr Mark Dweck at Edinburgh University on the EVOLVED Aortic stenosis study. This multicentre study being conducted in the United Kingdom evaluates the role of cardiac magnetic resonance imaging in patients with severe asymptomatic aortic stenosis compared to standard treatment. As well as multicentre collaborative work we have a number of advanced imaging research projects underway:
Transvalvular pressure drop estimation in aortic stenosis using novel MRI and echocardiographic techniques
Dr Harminder Gill, Dr Ronak Rajani, Dr Pablo Lamata
The mainstay of objective diagnosis and grading of aortic stenosis severity relies upon non-invasive assessment using echocardiography (ultrasound scans of the heart). One of these metrics in current clinical practice is the assessment of a pressure drop (referred to as a “pressure gradient” in guidelines) which is estimated using continuous wave Doppler echocardiography from the peak velocity of the blood flow across the valve. Using heavily devolved physics, the pressure drop (the simplified Bernoulli – SB – principle) can be calculated from this single peak velocity value (or the averaged values during the systolic interval). Where there is uncertainty over diagnosis, further investigations are undertaken but there are instances where the severity of aortic stenosis remains difficult to quantify or there are discrepancies between measured values. Therefore, clinical situations arise where a more accurate and reproducible measure of the severity of aortic stenosis may be able to better inform clinicians making decisions over valve replacement.
In conclusion, the overarching aim is to better characterize the severity and classification of aortic stenosis manner using 4D MRI flow patterns. The secondary aim is to determine the factors influencing these MRI flow profiles.
The hypothesis to be tested
The idea is to improve the velocity-based assessment of the pressure drop, expanding on the clinical evidence built upon during the last 30 years due to its availability (an echo exam). The team has discovered and solved a fundamental limitation of this approach using magnetic resonance imaging (MRI), and generated the evidence that a more accurate and precise assessment is possible. The hypotheses are thus:
1. An MRI-based assessment of AS severity better correlates with established indicators of aortic stenosis severity than the current clinical echocardiographic assessment of the peak pressure drop (as derived from the peak jet velocity using Simplified Bernoulli).
2. An MRI-based assessment of AS severity changes the stenosis severity classification of at least a 20% of the patients with respect to current clinical echocardiographic assessment.
In the project we will also investigate the feasibility of translating some of the MRI methodology to echocardiography. We thus hypothesize that it is possible to obtain an improved echocardiographic assessment of AS severity (and test equivalent hypotheses to H1 and H2) by capturing data of the velocity profile at the point of maximum constriction and applying the physics described in the Navier-Stokes equations as done in our preliminary work.
Optimization of pre- and post-procedural patient assessment for transcatheter heart valve replacement using personalised computer modelling
Samuel Hill, Ronak Rajani, Adelaide de Vecchi
In a rapidly ageing population, the prevalence of clinically significant valvular heart diseases is estimated to double by 2050, with mitral regurgitation the second most frequent condition after aortic stenosis. These forecasts carry serious implications for device makers and healthcare providers, who will be addressing the needs of a growing cohort of patients too old and frail for surgery. Following the success of transcatheter aortic valve implantation for patients at high surgical risk, this technology has recently been applied to mitral valve replacement. Both procedures offer a promising alternative to open-heart surgery, however new unique challenges have emerged in preprocedural planning due to the heterogeneity of the valve apparatus and the variety in design of the bioprosthetic valves. Choosing the correct device for each patient is crucial for the success of the procedure. Such key issue is yet to be addressed by imaging alone. Personalised computational modelling of the left ventricle with different types of bioprostheses has the potential to fill this knowledge gap by simulating the response of the left ventricle to implantation with different models, sizes, and positioning of the device.
Modelling surgical procedures to better understand both pathophysiology and treatment is a central research interest of the first supervisor, Dr Adelaide de Vecchi, who has a computer modelling background focussed on personalised modelling of the heart based on clinical imaging. Over the last three years she has been actively collaborating with the clinical team that performs cardiac valve replacement and repair at St Thomas’ Hospital. This team includes the second supervisor, Dr Ronak Rajani, who is a radiologist with a specialist interest in valvular diseases. On the topic of transcatheter valve replacement, Dr de Vecchi has published several peer-reviewed papers in collaboration with this team and has been involved in collaborations with valve manufacturers (Edwards, Medtronic) initiated by Dr Rajani1-4. These contributions resulted in the development of a methodology to perform patient-specific simulations of transcatheter mitral valve replacement using simplified models. This modelling platform is now ready to be enhanced by including more sophisticated models of both the bioprosthetic valve and the left ventricle. This work stemmed from the involvement of Dr Rajani in the Medtronic Intrepid Global Pilot study, for which St Thomas Hospital is a recruiting site. This clinical collaboration has been pivotal for obtaining patient datasets for personalising the models, as well as for understanding the clinical needs and challenges in the operating theatre, which are the main motivation for this study.
1. de Vecchi et al. EClinicalMedicine, 2018 6:9-10.
2. de Vecchi et al. Nature Scientific Reports. 2018 8:15540.
3. de Vecchi et al. International Journal Cardiovascular Imaging, 2018;34(5):803-805.
4. de Vecchi et al. Contribution to Chief Medical Report 2018.
This project will use image-based personalised models of left ventricle coupled to models of commercial bioprostheses to test the following primary research question:
Can computer models integrating patient-specific ventricular motion and haemodynamics with bioprosthetic design be used to guide the choice of the type, size and positioning of the device to be implanted?
Specifically, we will test the following research hypotheses:
The valve study group has a long history of evaluating heart valves and their durability and have conducted long term studies on the Cryolife O’Brien, Toronto, Perimount and On-X heart valves. In recent years we have been at the forefront of testing and evaluating new transcathter heart valves for aortic valve replacement (TAVI) and also mitral valve replacement (TMVR). This has included the world’s first in-human TMVR device, The world’s first LOTUS valve in mitral valve calcification and the world’s first SAPIEN 3 in mitral annulus calcification with fluroscopy and computer simulation guidance. Professors Prendergast, Redwood and Dr Rajani have been involved in the following new product trial evaluations:
A new clinic has been set up to evaluate patients with inoperable mitral valve disease ...
Read the full article >The Valve Research team are working with our partners at King’s College London (Dr Karabelas ...
Read the full article >International TAVI Congress - The Aortic Valve Meeting
Edinburgh, Scotland